The Evolution of Thymectomy
The evolution of thymectomy as a treatment for Myasthenia Gravis (MG) in the last 75 years is a fascinating chapter in medical history. It was not originally founded on strict scientific evidence but developed through clinical experience and anecdotal reasoning. The early surgeons who performed this procedure were strongly convinced of its effectiveness, even without systematic evidence to support their claims at that time. This lack of tangible proof on the part of doctors inevitably created suspicions among many physicians. Despite skepticism, thymectomy found acceptance with optimism, extending a glimmer of hope to thousands of patients struggling with this intractable and tricky disease.
Thymectomy has now been a pioneering treatment approach for non-thymomatous myasthenia gravis (MG). Current research identifies its amazing clinical benefits, such as reducing hospitalizations and the need for immunosuppressive drugs like prednisone, advances that have significantly enhanced the lives of patients. Another improved option is the extended thymectomy, in which not only is the thymus gland excised but also the surrounding mediastinal tissue. Evidence suggests that this more comprehensive approach produces better results than less intense methods. This has led clinicians to reconsider and revise traditional treatment protocols, ushering in better care.
Thymectomy is now a game-changer for patients with myasthenia gravis (MG), having a real impact not only on those who need to endure the condition but also on the healthcare system. Through its sharp reduction of hospitalization time during MG exacerbations, thymectomy has changed the way we treat the condition. Patients undergoing the procedure also reported a reduced need for medication like prednisone, meaning fewer side effects and overall better quality of life. As one study shows, "The patients treated with thymectomy had fewer hospitalizations for exacerbations and lower prednisone doses." (Joshua Sonett) Clearly, thymectomy is leading the way in improving patient outcomes in MG.
Thymectomy is far from short-term relief; it provides incredible long-term benefits for patients with non-thymomatous myasthenia gravis (MG). From three years of observation, research has shown that patients who underwent the operation have substantially better clinical outcomes. This signifies the fact that thymectomy accomplishes far more than addressing the immediate issue, making a huge difference in the overall health and well-being of patients. According to one study, "Thymectomy improved clinical outcomes over 3 years in patients with non-thymomatous myasthenia gravis." (Joshua Sonett) Given such compelling evidence, thymectomy has become a significant treatment for the management of MG.
Thymectomy is a procedure that indeed wears its badge of honor in patients of all age groups, showcasing just how clinically useful it is. It's made great strides in helping younger patients below the age of 40 years and older patients beyond the age of 40, revealing that regardless of your age, it works. This proves that thymectomy is not only reserved for any given group—it's a therapy for patients of various ages. As the report says, "It was found to improve in age groups less than 40 and greater than 40" (Joshua Sonett), once more exemplifying its suitability and success for everyone.
For the surgical treatment of myasthenia gravis (MG), specifically the non-thymomatous form, extended or maximal thymectomy has become the gold standard surgical procedure. This is not just the excision of the thymus gland—it's an entire removal of all the surrounding mediastinal tissue too. And it's worth it! Studies show it leads to much better clinical outcomes than minimally invasive procedures. As one study goes, "An extended or maximal thymectomy involving all mediastinal tissue, including the discrete thymus gland, should be considered the standard of surgical care." This therapy sets the bar for effectively curing MG with surgery.
Research strongly confirms how well thymectomy works to improve patient outcomes. Thymectomy has been shown to help patients by significantly reducing hospital stays for disease flare-ups. It also reduces the need for medications like prednisone, making it easier to control the disease. As another study states, "Patients treated with thymectomy had fewer hospitalizations for exacerbations and required lower prednisone doses" (Joshua Sonett), showing just how much this surgery can cut down on the burden of dealing with the condition.
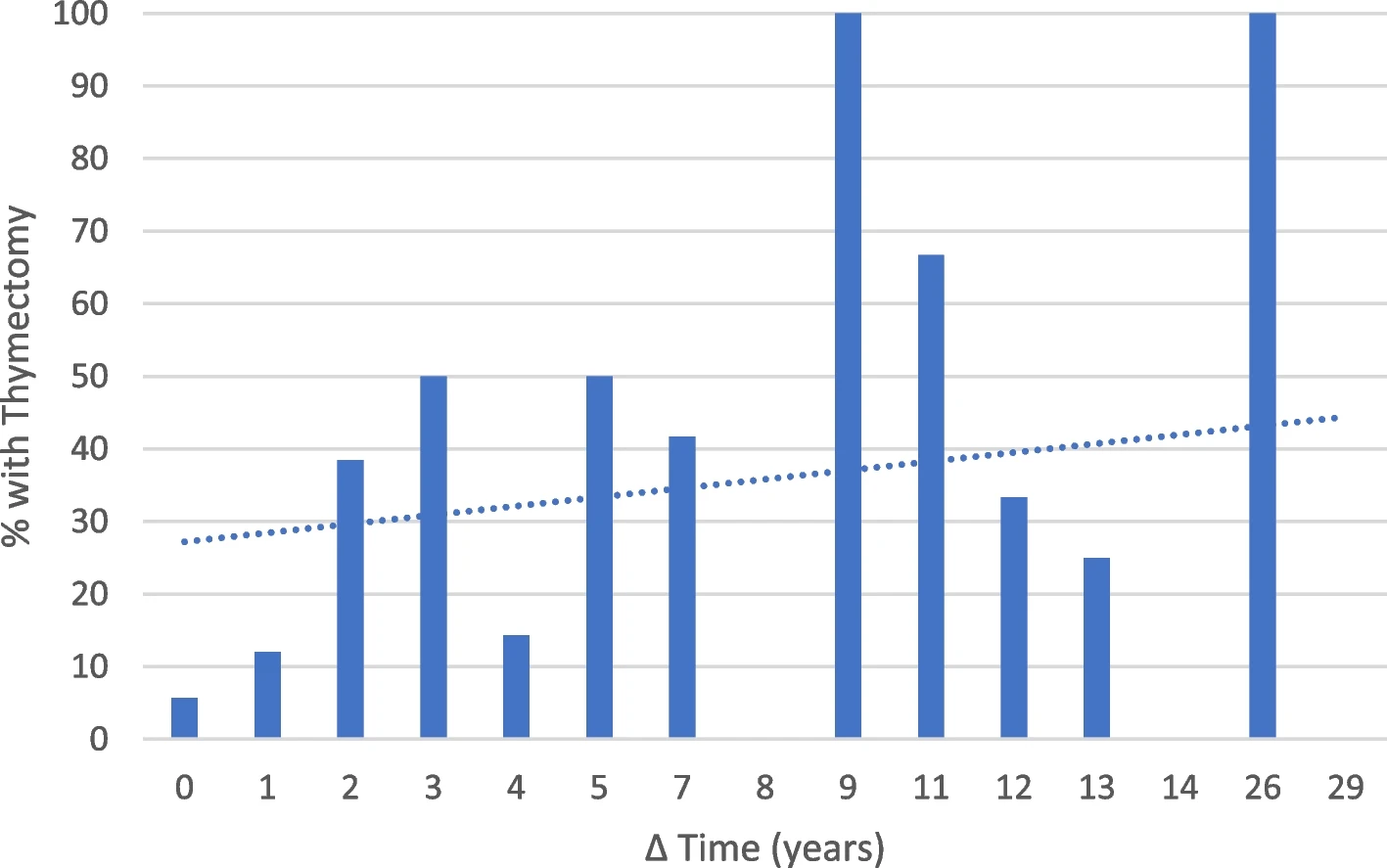
The research group studied three-year clinical outcomes in depth and discovered some impressive long-term benefits of thymectomy. As they succinctly put it, "Thymectomy improved clinical outcomes over a 3-year period in patients with non-thymomatous myasthenia gravis." (Joshua Sonett) This finding really highlights just how well the operation is at improving the quality of life in patients and solidifies its position as a required mode of treatment.
Extended thymectomy has proven to be phenomenally successful across a range of age groups, showing just how flexible this intervention is. Not only have younger patients younger than 40, but also older patients older than 40 have shown significant improvement, which testifies to its wide applicability. As the study mentions, "Improvements were noted in age groups younger than 40 and older than 40." (Joshua Sonett) This universality attests to its value as a standard treatment in the management of myasthenia gravis.
Aside from its clinical superiority, prolonged thymectomy also offers immense cost advantages in healthcare. By reducing the need for immunosuppressive drugs and decreasing hospital stay time, it is a cheaper form of treatment for MG in the long run. These favorable results have prompted clinicians to discard old surgical approaches and embrace this aggressive yet highly effective procedure as the treatment of choice.